Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
|
we as a country seem to have performed the hara-kiri that our cricket teams of the '80s and 90's were well known for. Before we had won the match, we started celebrating the victory, and seem to have lost the game. We didn't wait till Covid was completely under control. We started dismantling the specially created Covid Centers. We took our families to the malls and did not care about spraying sanitizers, before and after each interaction with something from outside our controlled environment. We started unmasking at will within our buildings and even at the Kirana stores. We started flying and driving around the country without masks and frolicking on the beaches of Goa. Our house parties were back on, and we destroyed the controlled zone that all India had worked so hard to become over a whole year. All, in less than a couple of months. And so it's back, worse than ever before, crippling our economy, our spirit, and making us feel bleak about the future. Except for this time, it doesn't look like everyone wants to tackle it together anymore. The center and the states don't seem to get along. The media is pushing up the pitch and the amplitude of the hyperbole. Strangely, vaccines seem to be running out. People are still not masking up. Many are demonstrating utter and complete stupidity with regards to bending the rules. Construction sites are working in full sway as if there is no covid in this world. Watchmen in buildings aren't sure if they should let delivery in or collect them at the gate, so they do nothing. And the poor Kirana-wala is feeling weird about asking the people coming to his shop to mask up again. My neighboring Kirana-wala told me he is not done arguing with customers who are say "khaasi pehle nahin hui kya" (Translates to "Haven't you had a cold before?") Sounds like March 2020 again! We both decided to formally put down our reasons for what has brought us to this stage. Policymakers must not let this happen again 1. The single biggest factor for the wave having arrived is how we have behaved in the recent past. 2. Mutating Strains: Not under control
3. The Vaccine rollout: Lessons to learn

|
Scooped by
nrip
|
India plans to spend a provisional sum of Rs 90,171 crore ($10.8 billion) for healthcare in the coming fiscal year, increasing from Rs 79,221 crore ($9.5 billion) previously. Some of it will go to the following key projects: - extension of the health assurance scheme, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana, to include 1.5 million community health workers called ASHA (accredited social health activist) and rural child care (Anganwadi) workers and helpers
- establishment of more medical and nursing colleges to help address the shortage of medical professionals
- the nationwide rollout of the U-WIN immunisation management platform and vaccination campaign to prevent cervical cancer among girls aged 9-14, which both contribute to Mission Indradhanush's goal of reaching 90% vaccination coverage of Indian children
- improved nutrition and better services by upgrading Anganwadi centres
- increased budget for biotechnology R&D to Rs 1,100 crore ($132.5 million) from Rs 500 crore ($60.2 million) in the previous year
Healthcare IT news speaks to industry leaders in this opinion piece https://www.healthcareitnews.com/news/asia/industry-seeks-clarity-indias-2024-tech-investment-health

|
Scooped by
nrip
|

|
Scooped by
nrip
|
The sudden second wave in the country left the government and the citizens in a fix. But ever since the second wave hit, the country has been constantly upgrading its healthcare system so that it can stand up to any challenge that comes next. Read on to know how India worked on its healthcare system. India’s April Covid hell brought immense agony. Close to 20% of all official deaths reported in India due to Covid-19, occurred over the four weeks of April. May brought dismay. While it’s a best-kept secret that the deaths were not being fully counted, the officially declared toll was 83,135. India’s “oxy-panic and distress made global headlines. The manic scramble for oxygen landed in courts, which told the central government “You can put your head in the sand like an ostrich, we will not." The distress created anger, which like a tsunami, dwarfed the Modi government's popular mandate of 2019. Aware the second surge had eroded the governement's political equity and a third could entail political calamity, the government prepared to battle the mutating pandemic and hostile opposition awaiting a political opportunity CHALLENGES BROUGHT CHANGE Did India change after the first two waves of the pandemic? Has adversity shaken off the seven decades of apathy towards building public health infrastructure? Through a series of review meetings starting March, Prime Minister Narendra Modi started a status check of decisions taken on availability of oxygen, ventilators, oxygen plants and other essentials since March 2020. ADVERSITY BROUGHT REMEDY The centre had started planning, ramping up the infrastructure in March-April 2020. Shortage of medical equipment like ventilators and cylinders was identified. Three companies were short listed to manufacture India-specific ventilators. Cut to 2021, the total number of ventilators is up to 57,557 from 16,644. Bulk of funds for this came from the PMCares fund, criticised by the opposition. OXYGEN AVAILABILITY & PREPAREDNESS As cylinders need refilling and facilities that can produce large amounts of Liquor Medical Oxygen were located in remote regions, the Centre keen to reduce the transportation time and upgrade availability, focused on creating local large, medium and micro-oxygen generation hubs. OXYGEN GENERATION PLANTS One of the key focus area for quick availability of oxygen in case of a crisis are PSA (Pressure Swing Adsorption) plants. The plants are being established in hospitals to enable them to become self-sufficient in generation of Oxygen. Under PM Cares, 162 PSA plants were sanctioned in 2020, out of which 77 are up and running and the rest will be on stream by July ’21. An additional 1,051 PSA Plants sanctioned under PM Cares Fund in March & April 21 are being procured through DRDO and CSIR and will be installed in the next three months in phases. This means by September, there will be over 1,200 oxygen plants up and running with the public health facilities. CRYOGENIC TANKERS To future-proof the public health system against a feared third wave, the government went in for capacity enhancement of Cryogenic tankers. LIQUID MEDICAL OXYGEN AVAILABILITY To ramp up oxygen supply for future production of Liquid Medical Oxygen (LMO), manufacturing was ramped up by more than 10 times from a paltry 900 MT/day in pre-Covid times to 9,300+ MT/day (as on 17th May 2021). At the current rate of production of 9,300 MT/day, India achieved the total LMO production of 2019 over in May. read more at https://www.indiatoday.in/coronavirus-outbreak/story/after-second-wave-has-india-upgraded-its-healthcare-system-for-next-big-challenge-read-to-know-1820077-2021-06-28

|
Scooped by
nrip
|
Digital Health has accelerated during the COVID-19 pandemic, enabling the health ecosystem, providers and patients to adopt new medical technologies and digital health solutions, specifically in remote patient care and telehealth. However, beyond addressing near-term pandemic issues, the full potential of digital health in tackling chronic care remains untapped.
To achieve this, we need to strike a balance between immediate priorities and investments for a digital future in a value-based care era. With a growing ageing population across the Asia-Pacific region and increased patient demand for access to care at a time and modality of their choice, digital health innovation is no longer an option, but a necessity for health systems if we aspire to emerge stronger from the pandemic.
It is for this reason that the Asia-Pacific Medical Technology Association (APACMed) formed the Digital Health Committee to drive proactive dialogue around key themes such as regulation, reimbursement, interoperability, and cybersecurity. The committee recently conducted an extensive research on Policy Pathways for Value Assessment and Reimbursement India and Australia were the two archetypes studied for the purpose of this research. Interestingly, for both archetypes studied – Australia (mature health system seeking to optimize UHC) and India (developing health system seeking to achieve “4.0” status), the core issues identified as part of the current landscape boiled down to policies that either inappropriately treat Digital Health as an unmonitored B2C platform, or the exact opposite - as a classic medical device. The three key challenges identified were, the lack of value assessment framework, fragmented coverage efforts and complex evidence generation.
Collectively, the efficacy of Digital Health can be improved to achieve the healthcare quality that our populations deserve, and simultaneously accelerate the time-to-market for innovations that will have wider socio-economic benefits. To begin this journey, it is critical to understand the unique socio-economic and health system challenges that countries in Asia Pacific could typically face.
India for instance, is a much younger population with only 6.4% aged above 65; the poverty rate steep and internet penetration lower (34.4%) in comparison to other developed nations. The healthcare system in India is still evolving with only 3.6% GDP allocation towards healthcare and only 30% for healthcare facilities supported by public entities. The country also has a very low ratio of doctors and beds per capita.
Incorporating Digital Health formally into the UHC (Universal Health Coverage) ambition in India will be very important especially considering COVID-19 and the challenges that it has been imposing on the country recently. read more at https://health.economictimes.indiatimes.com/news/health-it/harnessing-digital-health-in-asia-pacific/84059339

|
Scooped by
nrip
|

|
Scooped by
nrip
|
The pandemic accelerated the humanizing of digital technology – it brought people together at a time when physical distancing was legally mandated in many parts of the world. One year on, digital solutions – in every sector – have truly come of age. The pandemic has ushered in a new era and meaning for digital tech, as organizations, businesses, and institutions began to function through virtual mediums almost exclusively. Perhaps most crucially, it demonstrated just how powerful digital interventions can be in last-mile delivery of essential services, particularly in hard-to-reach, underserviced areas, and how they should be leveraged even in times of normalcy without such severe supply chain disruptions. Nowhere is this more apparent than in health care services. In the early months of lockdown in India, several essential health services were disrupted, and one of the hardest hit was maternal health care. Childbirth stops for nothing and no one – the ecosystem had to adapt almost overnight to meet the new challenges of maternal health care delivery. For instance, a quality improvement and assurance program called Manyata, which trains health care staff in private maternal care facilities on a set of 16 evidence-based clinical standards for quality and safe care, moved its entire training and certification architecture online to continue providing this crucial capacity-building to under-resourced nursing homes. And thus, digital interventions came to the rescue. With the immediate challenges of the pandemic addressed by a plethora of digital innovations, we must retain this momentum to chart a path for realizing India’s Universal Coverage Health goals. The digital ecosystem offers path-breaking and efficient solutions for accelerating the three pillars of UHC – availability, affordability, and quality – by advancing transformations in health care on both the demand and supply side. Digital tech can be a game-changer. In terms of supply, it is enabling reach and scale at levels that were previously unimaginable. Digital solutions can increase the penetration of quality care mechanisms to remote parts of the country through telemedicine and remote training sessions for health care staff. On the demand side, tech has tremendous potential to amplify grassroots voices from beneficiaries and patients, both as a means to incorporate their feedback in designing healthcare solutions (or improving existing ones), and encouraging demand for affordable, high-quality care. However, while leveraging digital interventions for improving healthcare and service delivery is crucial, it cannot be done in silos. The pandemic has exposed fragilities in the very foundations of our healthcare ecosystem. We must therefore create strong structural support that can enable availability, affordability, and quality to become all-pervasive, by rallying the health ecosystem and incentivizing the participation of both private and public sector. Perhaps most crucially, the private sector needs to be integrated into the total health system in order to complement and augment government efforts in strengthening the health care ecosystem. The important role of the private sector was amply reinforced in the aftermath of the Covid-19 pandemic, as the government turned to private sector facilities to help in its frontline response to the virus. So, too, with building a digitally-enabled health ecosystem. The visionary National Digital Health Mission (NDHM) is poised to revolutionize Indians’ experience of health care access and delivery. However, for the NDHM to achieve scale and speed of impact, extensive private sector involvement is crucial. A strengthened and integrated health system must put its weight behind digital interventions if we hope to facilitate a transformation in the months and years ahead. read the original , unedited version at https://timesofindia.indiatimes.com/blogs/voices/digital-technology-the-next-frontier-in-healthcare-delivery-in-post-covid-india/

|
Scooped by
nrip
|
India, being a huge country, has always suffered from lack of universal access to quality healthcare. As a result, a huge chunk of healthcare needs end up being unmet. However, with the increased proliferation of information technology in the healthcare industry, access to healthcare has been positively influenced. Healthcare is now accessible at our fingertips in the form of online appointments, online consultations, online delivery of medicines, etc. However, this digital avenue also requires the government to lay down the appropriate legal framework to prevent misuse of technology and exploitation of the end customer/user. Even though there has been an honest attempt at regulating the online healthcare industry by the authorities, the current regulatory regime is a hit and miss. The regulatory clarity around the e-healthcare industry does not extend to the e-pharmacy industry, because of which the last mile connectivity of the e-healthcare industry is severely affected. E-pharmacies have been caught in a regulatory quagmire ever since they first started operating in the country. The need of the hour is to put in place a comprehensive framework for digital healthcare in India which takes into its fold all its key components. Online delivery of medicines cannot be divorced from online consultations and therefore, a standardised regulatory regime needs to be set up to provide clarity to all the stakeholders in this industry. The regulatory initiatives relating to online consultations such as the Telemedicine Guidelines, EHR Guidelines, etc. also need to be extended to online pharmacies to instil confidence in major market players. read the entire article at https://www.mondaq.com/india/healthcare/1063794/digital-healthcare-in-india-a-need-for-standardisation

|
Scooped by
nrip
|
India features close to the bottom in international rankings in most health indices. The Covid-19 pandemic has exposed the fundamental problems plaguing the healthcare system, be it physical infrastructure, manpower or health management. At least two-thirds of India’s 1.3 billion people depend on the public healthcare system, but the country has only 8.5 hospital beds and eight physicians per 10,000 people. On account of the burgeoning costs of private healthcare and the inability of public healthcare to respond to the needs of the huge population, India’s remote villages have been traditionally relying on indigenous health systems of basic care supported by community agents. Community health workers are greatly improving the life of millions of people where doctors and nurses don’t go. Community healthcare providers, like paramedics, are taught essential services such as maternal and child healthcare. The strategy is to move beyond doctors and nurses and shift down to lay people, peers and family. An Accredited Social Health Activist — or ASHA, an acronym that translates as “hope” in Hindi — is the Government’s recognised health worker who is usually the first port of call for any health-related demands in rural India, where healthcare facilities are scant and medical professionals can be hard to find. As a result, many Indian communities, especially women and children, rely on ASHAs for primary healthcare. In many villages there are 1,000 to 1,500 people in each ASHA’s care. Any visitor to a village where these community healthcare models are the primary drivers of awareness will marvel at the ability of the ASHAs to connect with and explain things to women. Their lack of a degree is not a handicap, it is an advantage. They understand how to reach the people who most need reaching out to: The illiterate, vulnerable and poor village women. They know how they think and live, because they are one of them. The efficacy of the ASHAs can be seen in the impact they have made on India’s healthcare indicators. Their efforts have contributed to a 59.9 per cent decline in maternal mortality and a 49.2 per cent decline in infant mortality. Under their aegis, immunisation rates for the country increased from 44 per cent to 62 per cent and institutional deliveries doubled from 39 per cent to 78 per cent. While ASHA workers have the potential to play a wider role in rural healthcare, their service conditions are pathetic and need to be improved read the original unedited article at https://www.dailypioneer.com/2021/columnists/ashas-need-a-ray-of--hope-in-their-lives.html

|
Rescooped by
nrip
from The NDHM Blog
|
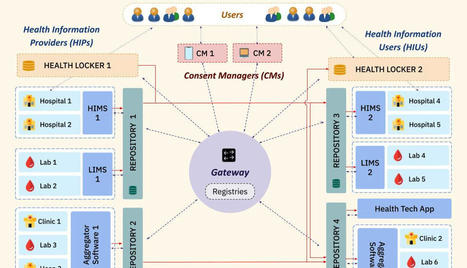
NDHM Architecture NDHM is employing a federated architecture for its ecosystem. That means that management and data access occurs in a federated manner where different entities or systems will manage the health data.
There is no central data storage controlling and storing data.
Using the Federated Health Records Framework (FHR), patients can access and view their health records, and provide consent to any HIPs and HIUs to access their data.
To ensure smooth consented data sharing and time-bound data access, it is necessary to make the data traceable and auditable. Therefore the FHR Framework architecture leverages MeitY's Data Empowerment and Protection Architecture (DEPA) electronic consent framework, which is already being used in the financial sector. Here are some interesting technical features of the NDHM ecosystem FHIR for all Medical Data Asynchronous APIs Patient Privacy & Security Features of NDHM - HIPs can only create data if authorized by the Patient: - An HIU(Health Information User) can only get past health records of other HIPs if consented by Patient - Peer to Peer Data Transfer Between HIP & HIU Final Thoughts It is one thing to have a concept and another thing to implement and execute it. So far NDHM seems to be going in the right direction. And there is hope that it will continue to do so.
Technology is being given equal importance to gain the trust of all players involved in this industry.
Privacy and Security have been a prime priority in the project as you can see from the above article, this is an oft-ignored aspect in old projects. Hope it continues to stay this way. read the whole article at http://technology4doctors.blogspot.com/2021/05/an-overview-of-ndhms-technology.html

|
Scooped by
nrip
|
In India, two simulation exercises were conducted in Uttar Pradesh to - identify bottlenecks
- address possible challenges
- ensure a smooth #COVID19 vaccine roll-out in the largest state of the country
Vaccinating a large group of people is not easy, but the largest state of the country – Uttar Pradesh – prepared well for this task. With more than 200 million people residing in it, having conducted numerous vaccination campaigns in the past, preparing the health system to vaccinate its people was not new to the state government. However, to ensure smooth running of the much anticipated COVID vaccination introduction involving adult populations when the disease is still spreading, two dry runs were conducted in all 75 districts: one on January 5, 2020 in 853 sites and the other on January 11, 2020 at 3081 sites. Among these sites, half were in urban and the other half in rural areas in first dry run. This is the kind of planning and execution strategy which is part of the success of India's COVID Vaccination program. Well done India Read the mid-planning phase post about this on the WHO Website https://www.who.int/india/news/feature-stories/detail/preparing-the-largest-state-health-system-for-covid-vaccine-introduction-an-update-from-uttar-pradesh

|
Scooped by
Plus91
|
India is one of the world’s largest democracies and the way it makes a mark on the global map being a powerful and emerging economy, it gives positive insight about the future prospect of the country. Healthcare, being India’s one of the largest sectors both in terms of revenue and employment, has witnessed a huge transformation in the last decade. The latest technology and innovative digital tools have led the Indian healthcare delivery system to get evolved in terms of providing enriched healthcare experience to masses especially in the front of clinical outcomes. With the Government undertaking many measures to bolster patient care and private players playing equally pivotal roles, the sector is making giant leaps to enable people at large to avail accessible and affordable healthcare. The healthcare sector is projected to become 8.6 trillion by 2022. The unprecedented growth of the healthcare sector is due to a range of factors including spike in non- communicable diseases, a considerable increase in income of the middle class, more awareness, quest for quality care, and easy access to service providers. The government also seems to be determined to provide quality health for all. With this objective, the spending is set to be increased to 2.5% of the gross domestic product by 2025. Even though the healthcare sector is growing, there is low accessibility and affordability for most of the population as the insurance coverage is less plus the costs of healthcare are also rising. Some of the biggest factors for limiting healthcare accessibility include:- 1. We have 7 beds for 10,000 population whereas globally it is 26 beds. 2. There are more medical professionals in the urban area than in the rural areas/villages where a large strata of our population lives with low accessibility to healthcare. 3. The insurance coverage is also very low as compared to other countries leading to an increase in out-of-pocket expenditure taking a toll on the patients. 4. There is a shift in disease patterns from communicable to non- communicable diseases like diabetes and cardiovascular disorders. The cardiovascular diseases are the highest known cause of death especially in the younger age group in India. The way technology is making an impact, the time has come when just doctor-patient engagement is not enough. With continuous technological growth, the healthcare industry is going to be more based on “Value-based care “ outcomes in the coming days. New trends as per Vision2024 would be– 1. Healthcare will go mobile.
2. New strategies to deliver low-cost healthcare will be on the rise.
3. New drug pricing models will be unveiled.
4. Behavioral healthcare will see more acceptance.

|
Scooped by
Plus91
|
In a breakthrough in research, IIT-Bombay scientists have developed technology to leverage a patient’s immune system to cure cancer. Researchers made use of gene and cell therapies to reengineer immune cells to attack and kill cancer cells in the body. Such immunotherapy using CAR T-cells, a treatment for cancer, which costs Rs 3-4 crore in the US, can be made available for Rs 15 lakh if the technology is developed in the country. Purwar's team has been working on CAR T-cell technology for six years. ''It is an autologous cell therapy for personalized medicine, where cells are taken from patients, re-engineered and re-infused in the patient. We got immune cells from volunteers and clinical patients with help from TMH and re-engineered them using the technique. The modified cells were positively tested in laboratories on artificially grown cancer cells.'' said Purwar. T-cells (a type of white blood cell or WBC), an integral part of the human immune system, can identify tumors and destroy them. But in advanced stages, the cancer cells adapt to the presence of T-cells and remain undetected. In the new approach in immunotherapy, called CAR (chimeric antigen receptors) T-cell therapy, the T-cells ability to detect and kill cancer cells is restored. CARs are the protein that assists T-cells to recognize and attach to protein or antigen, present on cancer cells. These proteins help to destroy cancer cells. ''Our team has delved into strategies that would improve the efficacy of the technique and demonstrated that a single injected dose can lead to multiplication of modified T-cells that can destroy cancer cells,'' said Punwar. Globally, over 600 clinical trials are in progress for CAR T-cell therapy, many of which are on in China said, Dr. Narula from TMH. ''It has got huge potential. With the cancer burden, we have, the therapy will be considered a success, even if it is applicable to only a fraction of patients currently. Technologies are being developed globally, but are exorbitant. There are high expectations from this technology as it can create pathways for developing newer technologies, for newer therapies, for more forms of cancer. Thousands of Asians can benefit,'' said Narula. Read More: https://timesofindia.indiatimes.com/city/mumbai/iit-bombay-scientists-now-develop-cheaper-tech-to-cure-cancer/articleshow/72483167.cms
|

|
Scooped by
nrip
|
The CEO, of Lupin Digital Health, Sidharth Srinivasan, spoke with ETHealthworld. about how the perception of cardiac rehab is witnessing a significant shift. He spoke about the major insights and adoption trends registered over one year since the launch of their digital therapeutic platform Lupin's Lyfe. Summarizing their talk, he mentioned that the program has grown in 3 ways: 1. the acceptance of digital interventions has increased in the cardiology community. Over 700 cardiologists across 20 cities actively prescribe Lupin’s LYFE, our digital therapeutics, and more than 90 per cent of patients are satisfied with the service. 2. conducted and published real-world evidence studies, including two trials and two consensus statements. 3. LDH has been able to reach out to patients, with around 5000 patients signing up for months of rehab. His comments also shed light on some of their plans for the the future which included plans to conduct India's largest digital therapeutic study, involving around 1000 patients, to comprehensively showcase the impact of digital therapeutics on cardiac rehab. He mentioned that Lupin was actively utilising technology to simplify backend processes, among which was the use of AI to analyse patient reports. read the entire unedited version of interaction here: https://health.economictimes.indiatimes.com/news/pharma/pharma-industry/lupin-digital-health-planning-indias-largest-study-on-impact-of-digital-therapeutics-on-cardiac-rehab/108653359

|
Scooped by
nrip
|
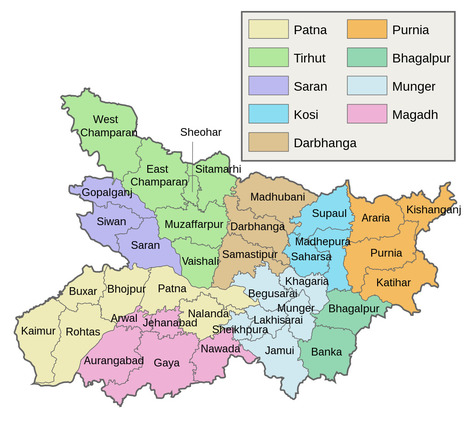
Mukhyamantri Digital Health Yojana (MDHY): Introduction of Mukhyamantri Digital Health Yojana (MDHY) in Bihar involves digitizing the state’s health system to improve healthcare services and ensure transparent governance. It will connect 13,000 public health facilities and 30,000 healthcare professionals, providing easy access to medical advice and services for citizens. The project utilizes the ‘BHAVYA’ Hospital Information Management System (HIMS) and centralizes healthcare data for enhanced transparency and efficiency. This initiative supports SDG 3 – Good Health and Well-being by digitizing the state’s health system, improving healthcare services, and providing easy access to medical advice and services for citizens. more at the source: https://timesofindia.indiatimes.com/blogs/blackslate-corner/in-national-multidimensional-poverty-index-2023-bihar-recorded-the-steepest-decline-in-number-of-mpi-poor/

|
Scooped by
nrip
|
Digital tools are increasingly being applied to support the response to the ongoing COVID-19 pandemic in India and elsewhere globally. This article draws from global frameworks to explore the use of digital tools in the state of Kerala across the domains of communication, surveillance, clinical management, non-clinical support, and core health system readiness and response. Kerala is considered India’s first digital state, with the highest percentage of households with computers (24%) and the internet (51%) in India, 95% mobile phone penetration, 62% smartphone penetration and 75% digital literacy. Kerala has long been a model for the early adoption of digital technology for education and health. As part of the pandemic response, technology has been used across private and public sectors, including law enforcement, health, information technology and education. Efforts have sought to ensure timely access to health information, facilitate access to entitlements, monitor those under quarantine and track contacts, and provide healthcare services though telemedicine. Kerala’s COVID-19 pandemic response showcases the diverse potential of digital technology, the importance of building on a strong health system foundation, the value of collaboration, and the ongoing challenges of data privacy and equity in digital access. Summary -
The COVID-19 pandemic’s unprecedented global spread and impact has accelerated interest in digital innovation. -
Kerala’s experience showcases the diverse and innovative ways that digital tools can build on a strong underlying health system to support pandemic response across the domains of communication, surveillance, clinical management, non-clinical support and core health system readiness. -
Digital tools in Kerala were able to proliferate rapidly and help meet diverse citizen needs due to high levels of collaboration and intersectoral response that brought together different levels of government and multiple state departments, engaged the private sector, and harnessed the energy of civil society organisations and community volunteers. -
Digital technology has great potential to strengthen public health measures during pandemics, including to rapidly link citizens to food and mental health support. -
Adequate oversight and community participation remains essential to safeguard citizen privacy and ensure equity. read the open access paper at https://gh.bmj.com/content/6/Suppl_5/e005355

|
Scooped by
nrip
|
Data analytics allows healthcare organizations to make smarter and more educated decisions directly enhancing the patient experience, even more so with access to real-time data. The potential for improving overall patient care, collaboration, and analysis with the aid of cloud technology and data analytics is enormous. As India is preparing for digitalization to harness the power of data, migration to cloud systems and use of data-driven solutions give healthcare organizations the flexibility and storage they need to handle such vast amounts of data, allowing them to gain insights that improve patient care and hospital operations. Healthcare staff and executives will be in a better position to make the right decisions that enhance overall care when they have access to real-time data. This will empower practitioners to deliver the highest quality care in hospitals of tomorrow. read more at https://health.economictimes.indiatimes.com/news/health-it/changing-the-future-of-healthcare-with-data-anlaytics/83811935

|
Scooped by
nrip
|
The second wave of COVID-19 was unrelenting on India's healthcare workers, hospitals, governments and citizens...

|
Scooped by
nrip
|
The state government of Haryana in northern India has kicked off a project with Deloitte to provide virtual home care services to patients with mild to moderate symptoms of COVID-19 amid the ongoing second wave of infections in the country. Sanjeevani Pariyojana, or The Life Project, provides patients with support and resources to manage their care at home, including access to virtual triage, COVID-19 field hospitals and in-patient facilities. It was piloted in the Karnal district before being expanded to other districts in Haryana. more at https://www.healthcareitnews.com/news/apac/indias-haryana-state-partners-deloitte-covid-19-virtual-home-care-service

|
Scooped by
nrip
|
A report by the World Health Organisation (WHO) reveals that patients living in low-income countries experience as many disability-adjusted life years lost due to medication related harm than those in high-income countries. For patients in hospital, the impact of clinical errors is greater, and this may be attributed to the complexity of certain diseases and the use of complicated medication regimes. In children and elderly, medication errors often occur due to administration of wrong dosage, incorrect therapeutic route and a failure if the patient does not follow the prescribed treatment.
The Crucial Role of Digital Tools for Better Patient Outcomes
Today, with the increase in disease profiles and the influx of information available across online mediums, there is a dire need to have a platform that can provide filtered, precise and reliable medical information. Moreover, as the pandemic has posed unprecedented challenges for the healthcare industry, the need of the hour is a database with different treatment types used for both non-communicable and communicable diseases. Considering this, digital healthcare technologies such as Clinical Decision Support (CDS) systems are providing healthcare professionals with innovative diagnostic and treatment solutions that enable them to deliver quality patient care.
CDS systems improve patient safety, discard unnecessary tests, reduce cost, and increase satisfaction of patients and clinicians. The platforms use biomedical information, patient-specific data or a mechanism that integrates knowledge and data to present useful information to the doctor when healthcare is delivered, enabling quicker action. All healthcare professionals and hospitals should use CDS systems that can provide them information that is verified by doctors who have years of experience. It is imperative to understand that clinical errors do not occur due to medical negligence, in fact they include a range of honest errors and innocent mistakes which are beyond the healthcare provider’s control, despite enough caution. We experienced an onslaught and sudden surge in use of healthcare technologies owing to the pandemic. In the post pandemic, the trend of virtual care is anticipated to grow even more that will ensure smarter and quality care. And when we say digital healthcare technologies are here to stay, the rationale is to not get rid of paper record, but to adopt more patient-centric methods. read the entire article at https://health.economictimes.indiatimes.com/news/industry/a-case-for-eliminating-medical-errors-with-evidence-based-decision-support/82818497
“ATMAN AI”, an Artificial Intelligence algorithm that can detect the presence of COVID-19 disease in Chest X Rays, has been developed to combat COVID fatalities involving lung. ATMAN AI is used for chest X-ray screening as a triaging tool in Covid-19 diagnosis, a method for rapid identification and assessment of lung involvement. This is a joint effort of the DRDO Centre for Artificial Intelligence and Robotics (CAIR), 5C Network & HCG Academics. This will be utilized by online diagnostic startup 5C Network with support of HCG Academics across India. Triaging COVID suspect patients using X Ray is fast, cost effective and efficient. It can be a very useful tool especially in smaller towns in India owing to lack of easy access to CT scans there. This will also reduce the existing burden on radiologists and make CT machines which are being used for COVID be used for other diseases and illness owing to overload for CT scans. The novel feature namely “Believable AI” along with existing ResNet models have improved the accuracy of the software and being a machine learning tool, the accuracy will improve continually. Chest X-Rays of RT-PCR positive hospitalized patients in various stages of disease involvement were retrospectively analysed using Deep Learning & Convolutional Neural Network models by an indigenously developed deep learning application by CAIR-DRDO for COVID -19 screening using digital chest X-Rays. The algorithm showed an accuracy of 96.73%. read more at http://indiaai.gov.in/news/drdo-cair-5g-network-and-hcg-academics-develop-atman-ai

|
Scooped by
nrip
|
The Global Fund has approved US$75 million in fast-track funding to support India’s response to the COVID-19 crisis that is devastating the country. This new funding will support India in purchasing oxygen concentrators and Pressure Swing Adsorption (PSA) oxygen plants to help meet the medium-term needs for medical oxygen. “What is happening in India can happen elsewhere,” says Peter Sands. “This is a warning that we cannot let our guard down. The emergence and rapid spread of more virulent variants highlights the importance of a global and comprehensive approach – including testing, treatments such as corticosteroids and medical oxygen, and vaccines – to fight this pandemic. No country is safe until we have COVID-19 under control everywhere.” read the release at the Global Fund website at https://www.theglobalfund.org/en/news/2021-05-06-global-fund-approves-usd75-million-for-india-covid-19-response/

|
Scooped by
nrip
|
India’s vaccine diplomacy gets a boost from the Quad
The leaders of Quad countries (Australia, India, Japan, USA) have decided to launch a mega vaccine initiative under which coronavirus vaccines will be produced in India for the Indo-Pacific region with financial assistance from the United States and Japan while Australia will contribute in logistical aspects. As per a joint statement, the vaccination capacity of India will be increased to produce 1 billion doses by 2022, Foreign Secretary Harsh Vardhan Shringla said it was decided that India's manufacturing capacity is something that is going to be leveraged to make US vaccines. "In today's context, it is one of the most important initiatives. We are talking about huge investments in creating additional vaccine capacities in India for exports to countries in the Indo-Pacific region for their betterment. This will undoubtedly boost India’s vaccine diplomacy efforts. India has been providing vaccines to developing countries around the world. So far 71 countries have received vaccines manufactured in India. A majority of these are developing countries which did not have adequate access to the vaccine. India’s vaccine diplomacy has won attention for its efforts to make vaccine availability more equitable. On the other end, there has been criticism that India is working outside the WHO’s COVAX initiative in supplying vaccines. This hypocritical talk has been rejected by India’s External Affairs Minister Subrahmanyam Jaishankar who has asked “Which one of these countries have said that while I vaccinate my own people, I will inoculate other people who need it as much as we do?” There is a lot the world should learn from India's initiatives against the pandemic and its holistic and altruistic approach against it. Even though many will claim it is doing good so as to enhance its presence in the region, those same people must learn that as per Indian culture, its good to do good and not be concerned about the fruits that the good work may bear. The benefits are not the effect but a side effect.

|
Scooped by
nrip
|
Via three separate circulars, the Insurance Regulatory and Development Authority of India (IRDAI) has directed all insurers to standardize the terms for all policies they underwrite. It has also directed them to include TeleMedicine as part of claim settlement of policy. It has directed insurers not to bracket costs associated with pharmacy and consumables and implants. It has also directed companies to simplify the wordings of terms and clauses of policies. Insurers to cover TeleMedicine The regulator has directed insurers to include TeleMedicine as part of medical consultation cover in health policies. This was done as the Medical Council of India has issued TeleMedicine practice guidelines in March 2020 enabling doctors to provide healthcare using TeleMedicine. The provision of allowing TeleMedicine shall be part of claim settlement of policy of the insurers and need not be filed separately with the authority for any modification. However, the norms of sub limits, monthly/ annual limits, etc., of the product shall apply without any relaxation.

|
Scooped by
Plus91
|
Here is where we have a huge problem. Ayushman Bharat does very little for primary healthcare. It has been announced that 1.5 lakh health and wellness centers will be set up, partly to deal with primary healthcare issues including NCDs – but, given the budgetary allocation of less than Rs 1 lakh percenter, this looks more like a very minor upgrading of the existing sub-centers and/or primary healthcare centers (PHCs). Similar and sometimes more ambitious upgrading, including the provision of some free medicines, has been attempted by a number of states in the past; but, for the most part, there has been no reversal of the trend towards a wholesale exit from public healthcare, especially in North India. There is now a substantial body of work that documents that, in many states, more than three-quarters of visits to primary care centers are to private providers – even though most of these providers have no medical qualification whatsoever. This is in part because the sub-centers are open intermittently and unpredictably, and doctors and nurses are often missing from the PHCs. It seems unlikely that small investments in these sub-centers and PHCs will change all that; the patients will probably continue to stay away, and therefore using these as the basis of outreach for NCDs and other public health interventions probably have limited potential. The obvious alternative is to make use of informal providers who do have access to the patient population. It should certainly be recognized that they have the potential to be a public health hazard, especially because they abuse antibiotics and steroids – which contributes to rising resistance. However, the policy response to this phenomenon has been mostly to declare these informal providers illegal and then to ignore their existence. This essentially deprives us of the primary tool for dealing with the very serious health problems that we are facing. We need to think of ways to integrate them better into the overall healthcare project and give them better incentives, which would be easier if they had something to lose. Based on this we suggest the following steps. Recognize and train informal healthcare providers. A randomized control trial that was carried out in West Bengal (published in Science, 2016) shows that training private sector informal healthcare providers to improve their performance (measured by sending them ‘fake’ patients) by a very significant amount. Based on that, West Bengal has already begun training many thousands of informal health providers. Develop a set of cell-phone-based checklists For treatment protocols for these practitioners to use, to react to the common symptoms they face. This is similar to what Atul Gawande has proposed for the United States (but much more basic). Develop a simple test that allows the government to certify these practitioners as health extension workers. Passing this test will allow them to deliver various public health interventions and perhaps be paid for participating in them. Moreover, evidence suggests that the patients are aware of the value of such certification and trust those certified more. Recognize those who are certified As the front line of defense against NCDs and malnutrition. Think of ways to reward those whose referral leads to the detection of a serious ailment. Enforce existing laws That makes it impossible for these practitioners to dispense high-potency antibiotics and steroids. This includes shutting down stores that violate the existing laws about who can prescribe what. At the same time, make it legal for informal providers to prescribe a range of less critical medicines, much like the nurses. Expand the number of MBBS doctors and trained nurses Coming out of the system and consider introducing some other intermediate degrees for practicing a limited range of healthcare. This is the model we had before Independence and the one that many other countries have adopted. In addition, it is not clear that the government should rely entirely on the private sector to deliver tertiary care within PMJAY. There are already complaints from the healthcare sector about the prices the Indian government is proposing, which might result in many hospitals opting out and others selectively refusing to deliver certain treatments (even if that is against the rules). PMJAY will probably relieve some of this pressure on these public hospitals. However, it still makes sense for the government to try to simultaneously improve the delivery of secondary and tertiary care in the public sector. Given that public hospitals will be able to bill their patients to PMJAY, which gives the public hospitals stronger reasons to compete with the private sector, it is a natural moment to expand this part of the government system. Therefore, we recommend, for secondary and tertiary care: • Build a second district hospital in every district headquarters outside the state capital. Once it is built and is operational, refurbish and modernize the existing district hospital and bring it to acceptable standards. Finally, it is very difficult to improve healthcare substantially unless we get the customers to demand better care (to fear antibiotics, seek out tests, and so on). This has to be a priority for any government. This is our final recommendation: • Carry out public health campaigns to raise the awareness of NCDs, immunization and the dangers of overmedication. Recent evidence suggests that entertainment-education may be a very powerful device in this regard. Read More: https://www.telegraphindia.com/culture/books/nobel-laureate-abhijit-banerjee-on-what-ails-india-s-healthcare-sector/cid/1711667
|



 Your new post is loading...
Your new post is loading...